One of the most troubling aspects of my job as a medical addiction professional reared its head last week as I entered the exam room for a follow-up visit with Gordon.*
Gordon has had a very successful career in banking. He is the 64-year old divorced father of three grown children who adore him. He is very witty, personable, and engaging.
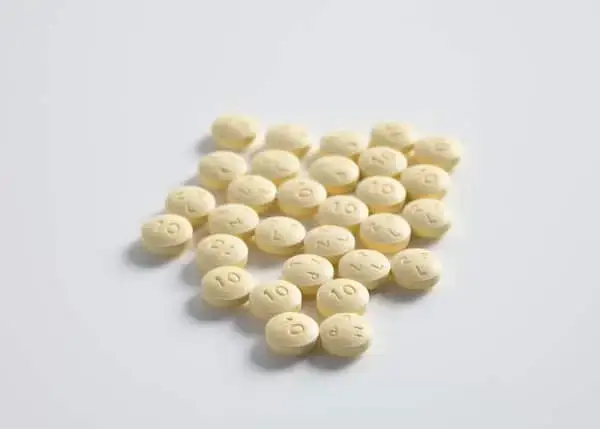
Close to twenty years ago, Gordon began seeing doctors about back pain. His back issues were not the result of a serious accident, but golfing and a gene pool of some lumbar instability combined to give him a pretty bad case of sciatica. While a little physical therapy was offered, doctors were quick to prescribe opioid pain medications. After all, this was believed to be the best treatment at the time.
A brief letter to the editor published in the New England Journal of Medicine in the 1980s is often cited as Ground Zero of the current opioid crisis. The author suggested that as long as a patient was in pain, it was safe to use opioid medication; addiction would not occur. Prior to this time, opioid medications were mostly restricted to acute severe pain conditions or terminal illness.
The amount of prescribing increased dramatically as doctors and other medical professionals began to use opioid medication for less acute and more chronic conditions. Patients began to expect they should be free of pain, rather than receiving help to control their pain.
Gordon, like thousands of others, fell squarely into this group. His doctors continued to prescribe, and his opioid medications made him feel good. He was able to not only function but thrive. He was a star in his profession, was in a satisfying second marriage, was an involved father and stepfather, and was able to golf several times a week.
He told me he occasionally had some ‘nagging doubts’ about being on chronic pain medications, but he was reassured by his doctors that it was safe, and it would actually be quite difficult to get off of them. For all he knew, his pain would return if he stopped the meds.
After about eight years of being on steadily increasing amounts of opioid pain medications, Gordon stopped kidding himself. He had no more–or very little—back pain; he knew he had a strong physical dependence on the medications, and he didn’t like it. He felt trapped.
This was about the time Suboxone® was being highly promoted and publicized as a solution for getting people off opioid pain medications, and his doctor, believing him to be an excellent candidate, switched him over. Gordon stayed on Suboxone® for ten years.
Ultimately, he wanted to be off this mediation as well, but after trying to stop on his own, he realized the degree of withdrawal involved. And with long-acting medications such as Suboxone® and methadone, the withdrawal can be quite protracted.
Gordon told me that he actually walked into—and then out of—the Coleman Institute office a full three times before he was brave enough to schedule a consultation to learn about an accelerated opioid detox.
He went through the detox with flying colors, as most people do, and he is dealing with the expected physical symptoms that often occur in the wake of a detox after almost 20 years of using opioid medications: mainly trouble sleeping and low energy.
Although we, the professionals who work with this condition daily, can reassure him that ‘this too shall pass’, and are helping him with some short term medications, Gordon is incredibly reluctant to take advantage of one of the most powerful aspects of the healing process: the camaraderie of being with other people who are going through, or have been through the same situation.
And here’s what’s bugging me:
The reason he doesn’t want to go to a recovery meeting is that he is so ashamed that he was on opioid medication for close to 18 years. He is worried he will see clients or friends and will be labeled and judged.
This makes me so sad for him because he truly was an innocent "victim" of his well-intentioned doctors. Once his body became physically dependent, getting off the medications would have been excruciatingly difficult. But Gordon sees this as a moral failing.
Dr. Brene Brown, author and social psychologist says, “ If we can share our story with someone who responds with empathy and understanding, shame can’t survive.” Although Gordon has obviously shared his story with our empathetic and understanding staff, my hope for him is that he can be as open with his children, and possibly with one of the many recovery support groups available to him.
I have no doubt he will get through the physical discomfort of early recovery, however, my real hope for Gordon and all of our patients, is to recognize the innocence of their role as people treated with opioids by well-intentioned, but inadequately informed medical professionals.
If you or a loved one is struggling with physical dependence on pain medication such as Nucynta®, Oxycontin®, hydromorphone, hydrocodone, tramadol, methadone, or buprenorphine; or have turned to street drugs such as heroin, fentanyl, or kratom, I hope you will give us a call 877-773-3869 to discuss an accelerated opioid detox. Please don’t let ill-placed shame keep you from reclaiming your life.
Joan R. Shepherd, FNP
*name and a couple of details changed to protect his privacy